Human societies have, from time immemorial, independently evolved and sustained systems of healing; Africans were not an exception. Despite efforts to suppress indigenous African medicine during and even after the colonial era the practice still thrives throughout the continent. The big question is whether there are prospects for complementary use of western and African medicine?
The World Health Organisation (WHO) defines traditional medicine as the sum total of knowledge, skills and practices based on the theories, beliefs and experiences indigenous to different cultures that are used to maintain health, as well as to prevent, diagnose, improve or treat physical and mental illnesses. Traditional African medicine and African religion are intricately intertwined; it is through African theology that illness, disease and misfortunes are understood.
Traditional African Medicine is a holistic discipline that embraces the use of herbs, African spirituality (diviner-healers), and traditional midwifery. African spirituality is centred on a belief in a supreme deity above a host of lesser semi-divine figures, including the power and intercession of ancestral spirits.
Normally, every rural African community will have a traditional healer, to whom they go for advice on a variety of issues, including health problems. The traditional healer would be knowledgeable about plant species that have medicinal value, including their ecology and conservation.
The philosophy underpinning traditional African Medicine differs significantly from that of western medicine. Whilst the latter is based on a system that focuses on identification of a specific disease-causing agent (germ theory), African medicine takes a holistic view. Good health, disease, success or misfortune, are seen as interrelated circumstances, which do not happen by chance but arise from the actions of living individuals or spirits of ancestors. Thus, the practice of traditional African medicine embraces the two mutually reinforcing elements of African spirituality (divination) and the use of herbs (herbal medicine).
Unlike in western medicine where the Hippocratic Oath obliges practitioners to be open with their modalities of treatment, absolute secrecy is what has sustained and protected the knowledge and mystery of traditional African medicine, through the ages. The gathering of medicinal plants is customarily restricted to the healers and their novices only, who normally will not divulge the nature of the plant, its environs and the details of its prescription to clients.
Christian missionaries were the indisputable ushers of western medicine in Africa. European and American missionaries pioneered ‘modern’ medicine in Africa, establishing health facilities deep into the interior way in advance of the colonial medical services.
Dr David Livingstone, the Scottish doctor and traveller, is recognized as the main source of inspiration for the involvement of Christian missions in medical work. His writings between 1851 and 1873 played a significant role in the recognition of medical care as an integral part of missionary activity. As a result, starting in the second half of the nineteenth and during the early twentieth century, mission hospitals, dispensaries and other medical facilities were established in West, East and Southern Africa[1].
Generally, Christianity was initially introduced at the Coast, before the missionaries penetrated the interior. By 1878, the White Sisters (Catholic Missionaries of Africa) had initiated health activities in the regions of the great lakes in East Africa. Among the earliest health facilities in East Africa were the Church Missionary Society (CMS) Hospital at Mengo, Uganda, established by Dr Albert Cook (1870-1951) in 1897, the Church of Scotland Mission (CSM) Hospital at Kikuyu, Kenya, in 1907, and the Africa Inland Mission (AIM) Hospital at Kijabe, Kenya, in 1915.

IMAGE: Mengo Hospital 1897
The arrival of the Christian missionaries provoked a cultural confrontation, especially when they completely ignored the existence of African spirituality. Influenced by their strong belief in the superiority of European culture, early missionaries viewed their primary mission to be that of exposing Africans to Western standards and practices, in other words, to ‘civilise the native’. In the mistaken belief that a spiritual vacuum existed in the lives of Africans, ready to be occupied by Western religion, they assumed that whatever forms of religion Africans subscribed to, could easily be supplanted by a superior religion, Christianity. They failed to distinguish between the roles, in the lives of Africans, of traditional culture and practices on the one hand, and of Christianity, on the other.
Professor John S. Mbiti, the pre-eminent African theologian and philosopher, has since exhorted that Christianity cannot afford to neglect, despise or even condemn outright, African traditional religions. Nor should the connection between African traditional practices and Christianity be seen as an “uncomfortable form of compromise”. He observes that in traditional African societies, religion and culture were completely integrated into one holistic way of life so that there was no distinction between what was sacred and what was secular. He advocates that Christianity ought to be viewed as the “fulfilment of that, after which African religiosity, in all its richness, has groped”[2].
Establishment of colonial medical services in East Africa was largely driven by the needs of colonial service officials and the white settlers. This was particularly the case in Kenya where there were numerous, and increasing numbers of Europeans in the so-called ‘white highlands’. Second to be considered were Indian, on whom the colonials looked upon to cater for their needs. Lastly, the meagre services extended to Africans, generally targeted the employees in the colonial administration and labour in white settler farms. As though to absolve themselves of the guilt of not providing for the health needs of African communities, the colonials have been quoted as blaming the preoccupation of the natives with witchcraft: ‘It was almost impossible “to administer to a people so thoroughly riddled with witchcraft that no one could do anything with them because they refused to tell anything”’!
The earliest government hospital to be established in Kenya (in 1901) was the Native Civil Hospital (NCH), Nairobi. This 40 bed facility provided in-patient services for Africans, while outpatient services were availed at the Government Dispensary which was located along Government Road (now Moi Avenue), close to Kingsway Police Station (today’s Central Police Station). The NCH was the precursor to the King George VI (1952), later renamed, in 1964, the Kenyatta National Hospital.
For the large population of Africans, especially those who lived far from the urban centres where colonial medical health facilities never existed, it mostly fell on missionaries (and/or traditional healers) to provide the much needed health services. Even today church-based hospitals and health care programmes continue to account for 25 percent to 50 percent of available services in most African countries, including Kenya.
Enjoy the best of both worlds? Practitioners of western medicine have over the years, eschewed traditional African medicine dismissing its methods as primitive, superstitious and pagan. Besides herbs, some healers may involve in their treatments, charms, incantations, and the casting of spells (demons); others may employ music and dance as in the case of the Akamba kilumi.
Under colonial rule, traditional diviner-healers were outlawed being considered to be practitioners of witchcraft. Similarly, African religious practices and medicine were labeled sinful by white Christian missionaries, and as such use of traditional medicine was forbidden for followers. However, in more recent years, traditional medicine has become more accommodated, and practitioners of “modern” medicine have increasingly acknowledged that there is much to learn from certain aspects of traditional medical practices. Indeed even the World Health Organization (WHO) has a department that promotes traditional medicine.
In any case, this was bound to happen since in most African countries, the penetration of ‘modern’ medicine remains such that large populations lack access to it, due to its relatively high cost and the concentration of health facilities in urban centres. According to the WHO, in some African countries, as much as 80% of the population may depend on traditional medicine for primary health care. This, among other reasons, legitimizes the call for enhanced research into the various practices employed in African traditional medicine. Africa is endowed with many plants that can be used for medicinal purposes. In fact, out of the approximated 6400 plant species used for various applications in tropical Africa, more than 4000 are used as medicinal plants, used in the treatments of many varied diseases and illnesses[3].

Image Traditional healer
Faced with the mammoth challenge of making ‘modern’ health care services accessible to all, African governments have increasingly adopted policies in favour of integration of traditional African medicine into national health care systems. For example, in 2001, the African Union (AU) Summit of Heads of State and Government declared the period 2001–2010 as the Decade of African Traditional Medicine, and in 2003 adopted a plan of action for its implementation. In 2008, the Ouagadougou Declaration on Primary Health Care and Health Systems in Africa reiterated the Alma Ata Declaration by calling on countries “to set up sustainable mechanisms for increasing the availability, affordability and accessibility of essential medicines and the use of community-directed approaches and African traditional medicines”, among others.
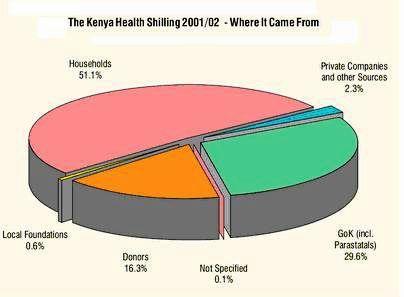
In countries, such as Kenya, governments have a constitutional obligation to facilitate the right of the citizen “to the highest attainable standard of health, which includes the right to health care services, including reproductive health care”[4].
However, it would be unfortunate (perhaps naïve?) to simply define healthcare in the context of ‘western’ medicine only. In fact, while still pursuing the ultimate goal of making healthcare available, accessible, affordable, and of good quality for all citizens, governments should be prudent enough to take the bold step (hard choice) of accepting the reality that a large segment of the population is already relying on traditional medicine.
There is evidence to show that traditional medicine and modern (western) medicine are quite frequently used complementarily, with traditional therapies serving as a first-line treatment before modern drugs are sought. For example, within certain communities in Kenya, majority of pregnant women will have consulted a mganga (traditional healer) who administered to them herbal preparations and potions to ward off evil spirits, before making their first antenatal clinic visit[5]. These women perceive antenatal care services obtained at health facilities, and those provided by TBAs and herbalists, to be complementary, and generally, they seek both types of care interchangeably.
The above is a strong reason why governments ought to establish appropriate regulatory mechanisms for accommodation of traditional medicine within the national health care system. Such a measure can go a long way towards assuring safety and effectiveness of the practice. A lesson may be learnt from the way traditional systems of medicine have been facilitated to grow in India and China, to the extent that today, leading institutions in the West are teaching and licensing practitioners of Ayurvedic medicine and Traditional Chinese Medicine.
However, a critical challenge for integration is sustaining the holistic concept of traditional African medicine, which traditionally embraced herbal medicine, divination and spiritual healing as mutually reinforcing systems, capable of dealing with physical, emotional and spiritual indispositions.
Whereas a considerable body of knowledge exists on herbal medicine, there is a dearth of scientific data on the other modalities of traditional medical therapy. This ought to be a challenge to African scientists, to engage with traditional medical practitioners, in the hope of establishing what is, and what is not practicable to integrate.
[1] H. J. O’D. Burke-Gaffney The History of Medicine in the African Countries http://www.ncbi.nlm.nih.gov/pmc/articles/…/pdf/medhist00144-0036.pdf
[2] Extract from a lecture given to the Christian Churches’ Educational Association of Kenya, 19 September 1969; see also J S Mbiti African Religions and Philosophy (London: Heinemann, 1969)
[3] Network on Medicinal Plants and Traditional Medicine (Eastern Africa). http://www.idrc.ca/EN/Resources/Publications/Pages/ArticleDetails.aspx?PublicationID=713
[4]The Constitution of Kenya, 2010 Article 43. (1)(a)
[5]Family Care International: Care-Seeking During Pregnancy, Delivery, and the Postpartum Period: A Study in Homabay and Migori Districts, Kenya, September 2003 http://www.familycareintl.org/UserFiles/File/SCI%20Kenya%20qualitative%20report.pdf